Mattson, C. L. et al. Developments and geographic patterns in drug and artificial opioid overdose deaths—United States, 2013–2019. MMWR Morb. Mortal. Wkly. Rep. 70, 202–207 (2021).
Gardner, E. A., McGrath, S. A., Dowling, D. & Bai, D. The opioid disaster: prevalence and markets of opioids. Forensic Sci. Rev. 34, 43–70 (2022).
Drug Overdose Deaths- NIDA. https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates.
CDC, Nationwide Middle for Well being Statistics, Workplace of Communication. U.S. Overdose Deaths In 2021 Elevated Half as A lot as in 2020—However Are Nonetheless Up 15%. cdc.gov https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm.
Matthes, H. W. et al. Lack of morphine-induced analgesia, reward impact and withdrawal signs in mice missing the mu-opioid-receptor gene. Nature 383, 819–823 (1996).
James, A. & Williams, J. Fundamental opioid pharmacology—an replace. Br. J. Ache. 14, 115–121 (2020).
Volkow, N. D. & Wargo, E. M. Overdose prevention by way of medical therapy of opioid use problems. Ann. Intern Med. 169, 190 (2018).
Volkow, N. D., Frieden, T. R., Hyde, P. S. & Cha, S. S. Medicine-assisted therapies—tackling the opioid-overdose epidemic. N. Engl. J. Med. 370, 2063–2066 (2014).
Dickson-Gomez, J. et al. “You’re Not Purported to be on it Ceaselessly”: drugs to deal with opioid use dysfunction (MOUD) associated stigma amongst drug therapy suppliers and individuals who use opioids. Subst. Abus. 16, 117822182211038 (2022).
Madden, E. F., Prevedel, S., Mild, T. & Sulzer, S. H. Intervention stigma towards drugs for opioid use dysfunction: a scientific evaluation. Subst. Use Misuse 56, 2181–2201 (2021).
Larochelle, M. R. et al. Medicine for opioid use dysfunction after nonfatal opioid overdose and affiliation with mortality: a cohort examine. Ann. Intern. Med. 169, 137 (2018).
Sullivan, L. E. & Fiellin, D. A. Narrative evaluation: buprenorphine for opioid-dependent sufferers in workplace follow. Ann. Intern. Med. 148, 662 (2008).
SAMHSA Drugs for Opioid Use Dysfunction. https://retailer.samhsa.gov/websites/default/recordsdata/SAMHSA_Digital_Download/PEP21-02-01-002.pdf.
Yamamoto, A. et al. Affiliation between homelessness and opioid overdose and opioid-related hospital admissions/emergency division visits. Soc. Sci. Med. 242, 112585 (2019).
Bateman, J. T., Saunders, S. E. & Levitt, E. S. Understanding and countering opioid‐induced respiratory melancholy. Br. J. Pharmacol. bph.15580 https://doi.org/10.1111/bph.15580 (2021).
Eliza Wheeler, T., Stephen, J., Michael Ok. G., Peter J. D., Facilities for Illness Management and Prevention (CDC). Opioid overdose prevention applications offering naloxone to laypersons—United States, 2014. MMWR Morb Mortal Wkly Rep. 64, 631-635 (2015).
Volkow, N. D. & Collins, F. S. The function of science in addressing the opioid disaster. N. Engl. J. Med. 377, 391–394 (2017).
Collins, F. S., Koroshetz, W. J. & Volkow, N. D. Serving to to finish habit over the long-term: the analysis plan for the NIH HEAL initiative. JAMA 320, 129 (2018).
Raleigh, M. D., Accetturo, C. & Pravetoni, M. Combining a candidate vaccine for opioid use problems with extended-release naltrexone will increase safety towards oxycodone-induced behavioral results and toxicity. J. Pharm. Exp. Ther. 374, 392–403 (2020).
Kimishima, A., Olson, M. E. & Janda, Ok. D. Investigations into the efficacy of multi-component cocaine vaccines. Bioorg. Med. Chem. Lett. 28, 2779–2783 (2018).
Stevens, M. W., Gunnell, M. G., Tawney, R. & Owens, S. M. Optimization of a methamphetamine conjugate vaccine for antibody manufacturing in mice. Int. Immunopharmacol. 35, 137–141 (2016).
Kosten, T. R. et al. Vaccine for cocaine dependence: a randomized double-blind placebo-controlled efficacy trial. Drug Alcohol Rely. 140, 42–47 (2014).
Cornuz, J. et al. A vaccine towards nicotine for smoking cessation: a randomized managed trial. PLoS One 3, e2547 (2008).
Hatsukami, D. Ok. et al. Immunogenicity and smoking-cessation outcomes for a novel nicotine immunotherapeutic. Clin. Pharm. Ther. 89, 392–399 (2011).
Bonese, Ok. F., Wainer, B. H., Fitch, F. W., Rothberg, R. M. & Schuster, C. R. Adjustments in heroin self-administration by a rhesus monkey after morphine immunisation. Nature 252, 708–710 (1974).
Pravetoni, M. & Comer, S. D. Growth of vaccines to deal with opioid use problems and cut back incidence of overdose. Neuropharmacology 158, 107662 (2019).
Alving, C. R., Matyas, G. R., Torres, O., Jalah, R. & Beck, Z. Adjuvants for vaccines to medicine of abuse and habit. Vaccine 32, 5382–5389 (2014).
Shen, X. Y., Orson, F. M. & Kosten, T. R. Vaccines towards drug abuse. Clin. Pharm. Ther. 91, 60–70 (2012).
Kimishima, A., Wenthur, C. J., Zhou, B. & Janda, Ok. D. An advance in prescription opioid vaccines: overdose mortality discount and extraordinary alteration of drug half-life. ACS Chem. Biol. 12, 36–40 (2017).
Hamid, F. A. et al. Pre-clinical security and toxicology profile of a candidate vaccine to deal with oxycodone use dysfunction. Vaccine 40, 3244–3252 (2022).
Bremer, P. T. et al. Growth of a clinically viable heroin vaccine. J. Am. Chem. Soc. 139, 8601–8611 (2017).
Belz, T. F. et al. Enhancement of a heroin vaccine by way of hapten deuteration. J. Am. Chem. Soc. 142, 13294–13298 (2020).
Hwang, C. S. et al. Heroin vaccine: utilizing titer, affinity, and antinociception as metrics when inspecting intercourse and pressure variations. Vaccine 37, 4155–4163 (2019).
Brisse, M., Vrba, S. M., Kirk, N., Liang, Y. & Ly, H. Rising ideas and applied sciences in vaccine growth. Entrance. Immunol. 11, 583077 (2020).
Baehr, C. et al. Preclinical efficacy and selectivity of vaccines focusing on fentanyl, alfentanil, sufentanil, and acetylfentanyl in rats. ACS Omega 7, 16584–16592 (2022).
Stone, A. E. et al. Fentanyl conjugate vaccine by injected or mucosal supply with dmLT or LTA1 adjuvants implicates IgA in safety from drug problem. NPJ Vaccin. 6, 69 (2021).
Crouse, B. et al. Efficacy and selectivity of monovalent and bivalent vaccination methods to guard towards publicity to carfentanil, fentanyl, and their mixtures in rats. ACS Pharmacol. Transl. Sci. 5, 331–343 (2022).
Frietze, Ok. M., Peabody, D. S. & Chackerian, B. Engineering virus-like particles as vaccine platforms. Curr. Opin. Virol. 18, 44–49 (2016).
Chackerian, B., Lowy, D. R. & Schiller, J. T. Conjugation of a self-antigen to papillomavirus-like particles permits for environment friendly induction of protecting autoantibodies. J. Clin. Investig. 108, 415–423 (2001).
Collar, A. L., Linville, A. C., Core, S. B. & Frietze, Ok. M. Epitope-based vaccines towards the chlamydia trachomatis main outer membrane protein variable area 4 elicit safety in mice. Vaccines 10, 875 (2022).
Jelínková, L. et al. A vaccine focusing on the L9 epitope of the malaria circumsporozoite protein confers safety from blood-stage an infection in a mouse problem mannequin. NPJ Vaccin. 7, 34 (2022).
Warner, N. L. & Frietze, Ok. M. Growth of bacteriophage virus-like particle vaccines displaying conserved epitopes of dengue virus non-structural protein 1. Vaccines 9, 726 (2021).
Tornesello, A. L., Tagliamonte, M., Buonaguro, F. M., Tornesello, M. L. & Buonaguro, L. Virus-like particles as preventive and therapeutic most cancers vaccines. Vaccines 10, 227 (2022).
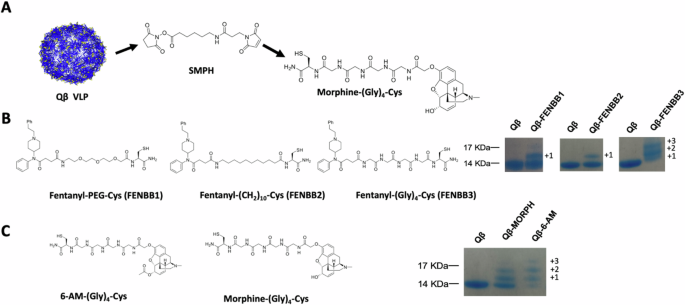
Romano, I. G. et al. A bacteriophage virus-like particle vaccine towards oxycodone elicits high-titer and long-lasting antibodies that sequester drug within the blood. Vaccine 42, 471–480 (2024).
Maphis, N. M. et al. Qß Virus-like particle-based vaccine induces strong immunity and protects towards tauopathy. NPJ Vaccin. 4, 26 (2019).
Peabody, D. S., Peabody, J., Bradfute, S. B. & Chackerian, B. RNA phage VLP-based vaccine platforms. Prescription drugs 14, 764 (2021).
Nooraei, S. et al. Virus-like particles: preparation, immunogenicity and their roles as nanovaccines and drug nanocarriers. J. Nanobiotechnol. 19, 59 (2021).
Martino, M. L., Crooke, S. N., Manchester, M. & Finn, M. G. Single-point mutations in Qβ virus-like particles change binding to cells. Biomacromolecules 22, 3332–3341 (2021).
Golmohammadi, R., Fridborg, Ok., Bundule, M., Valegård, Ok. & Liljas, L. The crystal construction of bacteriophage Q beta at 3.5 A decision. Construction 4, 543–554 (1996).
Selley, D. E. et al. μ Opioid receptor-mediated G-protein activation by heroin metabolites: proof for higher efficacy of 6-monoacetylmorphine in contrast with morphine 11Abbreviations: 6-MAM, 6-monoacetylmorphine; GTPγS, guanosine-5′-O-(γ-thio)-triphosphate; DAMGO, [d-Ala2,(NMe)Phe4,Gly5(OH)]enkephalin; M-6-G, morphine-6-βd-glucuronide; and hMOR-C6, C6 rat glioma cells expressing human μ opioid receptors. Biochem. Pharmacol 62, 447–455 (2001).
Maurer, H. H., Sauer, C. & Theobald, D. S. Toxicokinetics of medicine of abuse: present data of the isoenzymes concerned within the human metabolism of tetrahydrocannabinol, cocaine, heroin, morphine, and codeine. Ther. Drug Monit. 28, 447–453 (2006).
Bolger, G. T., Skolnick, P., Rice, Ok. C. & Weissman, B. A. Differential regulation of μ-opiate receptors in heroin- and morphine-dependent rats. FEBS Lett. 234, 22–26 (1988).
Sawynok, J. The therapeutic use of heroin: a evaluation of the pharmacological literature. Can. J. Physiol. Pharmacol. 64, 1–6 (1986).
Perekopskiy, D. & Kiyatkin, E. A. 6-Monoacetylmorphine (6-MAM), not morphine, is liable for the fast neural results induced by intravenous heroin. ACS Chem. Neurosci. 10, 3409–3414 (2019).
Gottås, A. et al. Ranges of heroin and its metabolites in blood and mind extracellular fluid after i.v. heroin administration to freely transferring rats: 6-MAM: a predominant metabolite of heroin. Br. J. Pharm. 170, 546–556 (2013).
Raleigh, M. D. et al. Opioid dose- and route-dependent efficacy of oxycodone and heroin vaccines in rats. J. Pharm. Exp. Ther. 365, 346–353 (2018).
Raleigh, M. D., Pentel, P. R. & LeSage, M. G. Pharmacokinetic correlates of the consequences of a heroin vaccine on heroin self-administration in rats. PLoS ONE 9, e115696 (2014).
Crossey, E. et al. A cholesterol-lowering VLP vaccine that targets PCSK9. Vaccine 33, 5747–5755 (2015).
Sato, Ok. et al. Environment friendly safety of mice from influenza A/H1N1pdm09 virus problem an infection by way of excessive avidity serum antibodies induced by booster immunizations with inactivated entire virus vaccine. Heliyon 5, e01113 (2019).
Bautista T. G. et al. The Brainstem Respiratory Community. In: Faingold CL, Blumenfeld H (Eds) Neuronal Networks in Mind Operate, CNS Problems, and Therapeutics. 235–245 (Tutorial Press, 2014).
Baldo, B. A. & Rose, M. A. Mechanisms of opioid-induced respiratory melancholy. Arch. Toxicol. 96, 2247–2260 (2022).
Tenney, R. D. et al. Vaccine blunts fentanyl efficiency in male rhesus monkeys. Neuropharmacology 158, 107730 (2019).
Shafieichaharberoud, F. et al. Enhancing protecting antibodies towards opioids by way of antigen show on virus-like particles. Bioconjugate Chem. 35, 164–173 (2024).
Pravetoni, M. Biologics to deal with substance use problems: present standing and new instructions. Hum. Vaccin. Immunother. 12, 3005–3019 (2016).
Hernández-Pérez, A. et al. Habit to tobacco smoking and vaping. RIC 75, 11315 (2023).
Oregon State College. Fentanyl Reality Sheet. https://oregonstate.app.field.com/s/7cxt86s4mqfu0miorqo3l7ouzxxvsfvy.
Benowitz, N. Medical pharmacology of nicotine: implications for understanding, stopping, and treating tobacco habit. Clin. Pharm. Ther. 83, 531–541 (2008).
Loud, E. E. et al. Hooked on smoking or hooked on nicotine? A spotlight group examine on perceptions of nicotine and habit amongst US grownup present people who smoke, former people who smoke, non‐people who smoke and twin customers of cigarettes and e‐cigarettes. Habit 117, 472–481 (2022).
Raleigh, M. D. et al. Pharmacological mechanisms underlying the efficacy of antibodies generated by a vaccine to deal with oxycodone use dysfunction. Neuropharmacology 195, 108653 (2021).
Pravetoni, M. et al. An oxycodone conjugate vaccine elicits drug-specific antibodies that cut back oxycodone distribution to mind and hot-plate analgesia. J. Pharm. Exp. Ther. 341, 225–232 (2012).
Bagley, S. M. et al. Incidence and traits of nonfatal opioid overdose amongst youths aged 11 to 24 years by intercourse. JAMA Netw. Open 3, e2030201 (2020).
Romanescu, M. et al. Intercourse-related variations in pharmacological response to CNS medicine: a story evaluation. JPM 12, 907 (2022).
Kest, B., Sarton, E., Dahan, A. & Fisher, D. M. Gender variations in opioid-mediated analgesia. Anesthesiology 93, 539–547 (2000).
Towers, E. B., Setaro, B. & Lynch, W. J. Intercourse- and dose-dependent variations within the growth of an addiction-like phenotype following extended-access fentanyl self-administration. Entrance. Pharmacol. 13, 841873 (2022).
Chan, S., Edwards, S. R., Wyse, B. D. & Smith, M. T. Intercourse variations within the pharmacokinetics, oxidative metabolism and oral bioavailability of oxycodone within the Sprague-Dawley rat. Clin. Exp. Pharm. Physiol. 35, 295–302 (2008).
St. John, A. L. et al. Novel mucosal adjuvant, mastoparan-7, improves cocaine vaccine efficacy. NPJ Vaccin. 5, 12 (2020).
Crouse, B. et al. A TLR7/8 agonist will increase efficacy of anti-fentanyl vaccines in rodent and porcine fashions. NPJ Vaccin. 8, 107 (2023).
Pravetoni, M. et al. Diminished antinociception of opioids in rats and mice by vaccination with immunogens containing oxycodone and hydrocodone haptens. J. Med. Chem. 56, 915–923 (2013).
Jones, D. I. et al. Optimized mucosal modified vaccinia virus Ankara prime/soluble gp120 increase HIV vaccination routine induces antibody responses just like these of an intramuscular routine. J. Virol. 93, e00475–19 (2019).
Haynes, B. F. et al. Immune-correlates evaluation of an HIV-1 vaccine efficacy trial. N. Engl. J. Med. 366, 1275–1286 (2012).
Lynch, H. E., Stewart, S. M., Kepler, T. B., Sempowski, G. D. & Alam, S. M. Floor plasmon resonance measurements of plasma antibody avidity throughout main and secondary responses to anthrax protecting antigen. J. Immunol. Strategies 404, 1–12 (2014).
Gårdmark, M., Höglund, A. U. & Hammarlund-Udenaes, M. Features on tail-flick, hot-plate and electrical stimulation exams for morphine antinociception. Pharmacol. Toxicol. 83, 252–258 (1998).