Bernal, W. & Wendon, J. Acute liver failure. N. Engl. J. Med. 369, 2525–2534 (2013).
Bernal, W. et al. Classes from look-back in acute liver failure? A single centre expertise of 3300 sufferers. J. Hepatol. 59, 74–80 (2013).
Sze, Y. Okay. et al. Pediatric liver transplantation for metabolic liver illness: expertise at King’s School Hospital. Transplantation 87, 87–93 (2009).
EASL Medical Follow Tips: Liver transplantation. J. Hepatol. 64, 433-485 (2016).
Asrani, S. Okay., Devarbhavi, H., Eaton, J. & Kamath, P. S. Burden of liver illnesses on this planet. J. Hepatol. 70, 151–171 (2019).
Adam, R. et al. 2018 Annual Report of the European Liver Transplant Registry (ELTR) – 50-year evolution of liver transplantation. Transpl. Int 31, 1293–1317 (2018).
Arulraj, R. & Neuberger, J. Liver transplantation: filling the hole between provide and demand. Clin. Med. 11, 194–198 (2011).
Dwyer, B. J., Macmillan, M. T., Brennan, P. N. & Forbes, S. J. Cell remedy for superior liver illnesses: Restore or rebuild. J. Hepatol. 74, 185–199 (2021).
Gadd, V. L., Aleksieva, N. & Forbes, S. J. Epithelial plasticity throughout liver harm and regeneration. Cell Stem Cell 27, 557–573 (2020).
Yovchev, M. I., Xue, Y., Shafritz, D. A., Locker, J. & Oertel, M. Repopulation of the fibrotic/cirrhotic rat liver by transplanted hepatic stem/progenitor cells and mature hepatocytes. Hepatology 59, 284–295 (2014).
Lu, W.-Y. et al. Hepatic progenitor cells of biliary origin with liver repopulation capability. Nat. Cell Biol. 17, 971–983 (2015).
Hallett, J. M. et al. Human biliary epithelial cells from discarded donor livers rescue bile duct construction and performance in a mouse mannequin of biliary illness. Cell Stem Cell 29, 355–371 (2022).
Forbes, S. J., Gupta, S. & Dhawan, A. Cell remedy for liver illness: From liver transplantation to cell manufacturing unit. J. Hepatol. 62, S157–S169 (2015).
Turner, R. A. et al. Profitable transplantation of human hepatic stem cells with restricted localization to liver utilizing hyaluronan grafts. Hepatology 57, 775–784 (2013).
Wang, Okay. et al. Overexpression of c-Met in bone marrow mesenchymal stem cells improves their effectiveness in homing and restore of acute liver failure. Stem Cell Res Ther. 8, 162 (2017).
Ma, H.-C. Focused migration of mesenchymal stem cells modified with CXCR4 to acute failing liver improves liver regeneration. World J. Gastroenterol. 20, 14884–14894 (2014).
Marcucci, Okay. T. et al. Retroviral and lentiviral security evaluation of gene-modified T Cell merchandise and infused HIV and oncology sufferers. Mol. Ther. 26, 269–279 (2018).
Naldini, L. Gene remedy returns to centre stage. Nature 526, 351–360 (2015).
Choi, G., Shin, G. & Bae, S. Worth and prejudice? The worth of Chimeric Antigen Receptor (CAR) T-cell remedy. Int J. Environ. Res. Public Well being 19, 12366 (2022).
Gu, Y. et al. Modular polymers as a platform for cell floor engineering: selling neural differentiation and enhancing the immune response. ACS Appl. Mater. Interfaces 11, 47720–47729 (2019).
Kim, Okay. S. et al. Native immune-triggered surface-modified stem cells for strong tumor immunotherapy. Adv. Funct. Mater. 29, 1900773 (2019).
Hwang, J. et al. Synthesis and characterization of purposeful nanofilm-coated stay immune cells. ACS Appl. Mater. Interfaces 10, 17685–17692 (2018).
Zhao, Y. et al. Floor-anchored framework for producing RhD-epitope stealth purple blood cells. Sci. Adv. 6, eaaw9679 (2020).
Moon, H. C. et al. Enzymatically degradable, starch-based layer-by-layer movies: utility to cytocompatible single-cell nanoencapsulation. Tender Matter 16, 6063–6071 (2020).
Kim, H. et al. Basic and facile coating of single cells through delicate discount. J. Am. Chem. Soc. 140, 1199–1202 (2018).
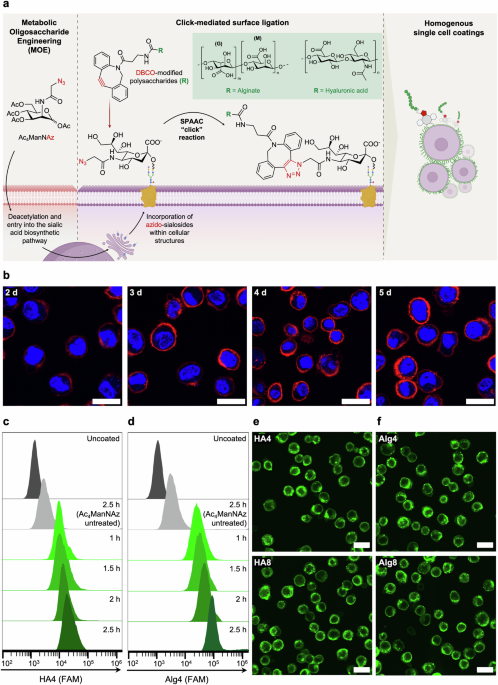
Mahal, L. Okay., Yarema, Okay. J. & Bertozzi, C. R. Engineering chemical reactivity on cell surfaces by way of oligosaccharide biosynthesis. Science 276, 1125–1128 (1997).
Saxon, E. & Bertozzi, C. R. Cell floor engineering by a modified Staudinger Response. Science 287, 2007–2010 (2000).
Prescher, J. A. & Bertozzi, C. R. Chemistry in dwelling methods. Nat. Chem. Biol. 1, 13–21 (2005).
Sletten, E. M. & Bertozzi, C. R. Bioorthogonal chemistry: fishing for selectivity in a sea of performance. Angew. Chem. 48, 6974–6998 (2009).
Sletten, E. M. & Bertozzi, C. R. From mechanism to mouse: a story of two bioorthogonal reactions. Acc. Chem. Res. 44, 666–676 (2011).
Soares Da Costa, D. et al. Bioorthogonal labeling reveals totally different expression of glycans in mouse hippocampal neuron cultures throughout their improvement. Molecules 25, 795 (2020).
Lee, S. et al. In vivo stem cell monitoring with imageable nanoparticles that bind bioorthogonal chemical receptors on the stem cell floor. Biomaterials 139, 12–29 (2017).
Prescher, J. A., Dube, D. H. & Bertozzi, C. R. Chemical remodelling of cell surfaces in dwelling animals. Nature 430, 873–877 (2004).
Wang, H. et al. Selective in vivo metabolic cell-labeling-mediated most cancers focusing on. Nat. Chem. Biol. 13, 415–424 (2017).
Mongis, A., Piller, F. & Piller, V. Coupling of immunostimulants to stay cells by way of metabolic glycoengineering and bioorthogonal click on chemistry. Bioconjugate Chem. 28, 1151–1165 (2017).
Nagahama, Okay., Kimura, Y. & Takemoto, A. Residing purposeful hydrogels generated by bioorthogonal cross-linking reactions of azide-modified cells with alkyne-modified polymers. Nat. Commun. 9, 2195 (2018).
Ono, Okay. et al. A skinny hydrogel barrier linked onto cell floor sialic acids by way of covalent bonds induces most cancers cell demise in vivo. Biomater. Sci. 8, 577–585 (2020).
Lavrador, P., Moura, B. S., Almeida-Pinto, J., Gaspar, V. M. & Mano, J. F. Engineered nascent dwelling human tissues with unit programmability. Nat. Mater. 24, 143–154 (2024).
Tchobanian, A., Van Oosterwyck, H. & Fardim, P. Polysaccharides for tissue engineering: Present panorama and future prospects. Carbohydr. Polym. 205, 601–625 (2019).
Wu, P., Xi, X., Li, R. & Solar, G. Engineering polysaccharides for tissue restore and regeneration. Macromol. Biosci. 21, 2100141 (2021).
Kesavan, Okay. Sodium alginate primarily based mucoadhesive system for gatifloxacin and its in vitro antibacterial exercise. Sci. Pharm. 78, 941–957 (2010).
Guarise, C. et al. The function of excessive molecular weight hyaluronic acid in mucoadhesion on an ocular floor mannequin. J. Mech. Behav. Biomed. Mater. 143, 105908 (2023).
Kim, H. et al. Mesenchymal stem cell 3D encapsulation applied sciences for biomimetic microenvironment in tissue regeneration. Stem cell res. ther. 10, 51 (2019).
Li, B. et al. Stiff hydrogel encapsulation retains mesenchymal stem cell stemness for regenerative medication. Matter 7, 3447–3468 (2024).
Vogel, J. et al. The function of glycolipids in mediating cell adhesion: a circulation chamber study1This paper is devoted to Professor H.W. Meyer (College of Jena) on the event of his sixty fifth birthday.1. Biochim Biophys. Acta 1372, 205–215 (1998).
Dafik, L., d’Alarcao, M. & Kumar, Okay. Modulation of mobile adhesion by glycoengineering. J. Med. Chem. 53, 4277–4284 (2010).
Iwasaki, Y., Matsunaga, A. & Fujii, S. Preparation of biointeractive glycoprotein-conjugated hydrogels by way of metabolic Oligosacchalide Engineering. Bioconjugate Chem. 25, 1626–1631 (2014).
D’Este, M., Eglin, D. & Alini, M. A scientific evaluation of DMTMM vs EDC/NHS for ligation of amines to Hyaluronan in water. Carbohydr. Polym. 108, 239–246 (2014).
Labre, F. et al. DMTMM-mediated amidation of alginate oligosaccharides geared toward modulating their interplay with proteins. Carbohydr. Polym. 184, 427–434 (2018).
Tomás, R. M. F. & Gibson, M. I. Optimization and stability of cell–polymer hybrids obtained by “Clicking” artificial polymers to metabolically labeled cell floor glycans. Biomacromolecules 20, 2726–2736 (2019).
Tomoda, H., Kishimoto, Y. & Lee, Y. C. Temperature impact on endocytosis and exocytosis by rabbit alveolar macrophages. J. Biol. Chem. 264, 15445–15450 (1989).
Nevi, L. et al. Hyaluronan coating improves liver engraftment of transplanted human biliary tree stem/progenitor cells. Stem cell res. ther. 8, 68 (2017).
Toole, B. P. Hyaluronan: from extracellular glue to pericellular cue. Nat. Rev. Most cancers 4, 528–539 (2004).
Garantziotis, S. & Savani, R. C. Hyaluronan biology: A fancy balancing act of construction, perform, location and context. Matrix Biol. 78-79, 1–10 (2019).
Tomás, R. M. F., Martyn, B., Bailey, T. L. & Gibson, M. I. Engineering cell surfaces by covalent grafting of artificial polymers to metabolically-labeled glycans. ACS Macro Lett. 7, 1289–1294 (2018).
Laughlin, S. T., Baskin, J. M., Amacher, S. L. & Bertozzi, C. R. In vivo imaging of membrane-associated glycans in growing zebrafish. Science 320, 664–667 (2008).
Gilormini, P. A. et al. Chemical glycomics enrichment: imaging the recycling of sialic acid in dwelling cells. J. Inherit. Metab. Dis. 41, 515–523 (2018).
Speicher, T. et al. Knockdown and knockout of β1-integrin in hepatocytes impairs liver regeneration by way of inhibition of progress issue signalling. Nat. Commun. 5, 3862 (2014).
Varol, M. Cell-extracellular matrix adhesion assay. Strategies Mol. Biol. 2109, 209–217 (2020).
Ricard-Blum, S. The Collagen Household. Chilly Spring Harb. Perspect. Biol. 3, a004978 (2010).
Adams, J. & Hohenester, E. Structural biology of laminins. Essays Biochem 63, 285–295 (2019).
Sano, Okay., Asanuma-Date, Okay., Arisaka, F., Hattori, S. & Ogawa, H. Modifications in glycosylation of vitronectin modulate multimerization and collagen binding throughout liver regeneration. Glycobiology 17, 784–794 (2007).
Giblin, S. P. & Midwood, Okay. S. Tenascin-C: Kind versus perform. Cell Adh Migr. 9, 48–82 (2014).
Lee, Okay. Y. & Mooney, D. J. Alginate: Properties and biomedical purposes. Prog. Polym. Sci. 37, 106–126 (2012).
JA, R., G, M. & DJ, M. Alginate hydrogels as artificial extracellular matrix supplies. Biomaterials 20, 45–53 (1999).
Baiocchini, A. et al. Extracellular matrix molecular transforming in human liver fibrosis evolution. PLOS ONE 11, e0151736 (2016).
Martinez-Hernandez, A. & Amenta, P. S. The extracellular matrix in hepatic regeneration. FASEB J. 9, 1401–1410 (1995).
Kostadinova, R. et al. Digital pathology with synthetic intelligence evaluation offers perception to the efficacy of anti-fibrotic compounds in human 3D MASH mannequin. Sci. Rep. 14 (2024).
Hay, D. C. et al. Extremely environment friendly differentiation of hESCs to purposeful hepatic endoderm requires ActivinA and Wnt3a signaling. Proc. Natl. Acad. Sci. U.S.A. 105, 12301–12306 (2008).
Zhang, H. et al. Restore of liver mediated by grownup mouse liver neuro-glia antigen 2-positive progenitor cell transplantation in a mouse mannequin of cirrhosis. Sci. Rep. 6, 21783 (2016).
Fagg, W. S. et al. Endoderm and hepatic progenitor cells engraft within the quiescent liver concurrent with intrinsically activated epithelial-to-mesenchymal transition. Cell Transpl. 30, 963689721993780 (2021).
Ho, C. M. et al. Transplantation pace presents early hepatocyte engraftment in acute liver injured rats: A translational examine with scientific implications. Liver Transpl. 21, 652–661 (2015).
Kultti, A. et al. Hyaluronan synthesis induces microvillus-like cell floor protrusions. J. Biol. Chem. 281, 15821–15828 (2006).
Shurer, C. R. et al. Bodily ideas of membrane form regulation by the Glycocalyx. Cell 177, 1757–1770 (2019).
Reiprich, S. et al. Adhesive properties of the hyaluronan pericellular coat in hyaluronan synthases overexpressing mesenchymal stem cells. Int. J. Mol. Sci. 21, 3827 (2020).
Yeung, T. et al. Results of substrate stiffness on cell morphology, cytoskeletal construction, and adhesion. Cell Motil. Cytoskel. 60, 24–34 (2005).
Du, J. et al. Integrin activation and internalization on delicate ECM as a mechanism of induction of stem cell differentiation by ECM elasticity. Proc. Natl. Acad. Sci. U.S.A. 108, 9466–9471 (2011).
He, M., Zhou, X. & Wang, X. Glycosylation: mechanisms, organic features and scientific implications. Sign Transduct. Goal Ther. 9, 194 (2024).
Guo, T. et al. Regulators, features, and mechanotransduction pathways of matrix stiffness in hepatic illness. Entrance. physiol. 14, 1098129 (2023).
Zong, Y. et al. Notch signaling controls liver improvement by regulating biliary differentiation. Improvement 136, 1727–1739 (2009).
Jo, M. H. et al. Single-molecule characterization of subtype-specific β1 integrin mechanics. Nat. Commun. 13, 7471 (2022).
Wang, X. & Ha, T. Defining single molecular forces required to activate integrin and notch signaling. Science 340, 991–994 (2013).
Dalton, S. L., Scharf, E., Briesewitz, R., Marcantonio, E. E. & Assoian, R. Okay. Cell adhesion to extracellular matrix regulates the life cycle of integrins. Mol. Biol. Cell. 6, 1781–1791 (1995).
Huet-Calderwood, C. et al. Novel ecto-tagged integrins reveal their trafficking in stay cells. Nat. Commun. 8, 570 (2017).
Dozynkiewicz, M. artaA. et al. Rab25 and CLIC3 collaborate to advertise integrin recycling from late endosomes/lysosomes and drive most cancers development. Dev. Cell 22, 131–145 (2012).
Lobert, V. H. et al. Ubiquitination of α5β1 integrin controls fibroblast migration by way of lysosomal degradation of fibronectin-integrin complexes. Dev. Cell 19, 148–159 (2010).
Blackman, M. L., Royzen, M. & Fox, J. M. Tetrazine ligation: quick bioconjugation primarily based on inverse-electron-demand diels−alder reactivity. J. Am. Chem. Soc. 130, 13518–13519 (2008).
Tomarchio, E. G. et al. Tetrazine–trans-cyclooctene ligation: Unveiling the chemistry and purposes inside the human physique. Bioorg. Chem. 150, 107573 (2024).
Younes, I. & Rinaudo, M. Chitin and chitosan preparation from marine sources. Construction, properties and purposes. Mar. Medication 13, 1133–1174 (2015).
Rossin, R. et al. Chemically triggered drug launch from an antibody-drug conjugate results in potent antitumour exercise in mice. Nat. Commun. 9, 1484 (2018).
Chang, M. et al. Bioorthogonal PROTAC prodrugs enabled by on-target activation. J. Am. Chem. Soc. 145, 14155–14163 (2023).
Li, H., Conde, J., Guerreiro, A. & Bernardes, G. J. L. Tetrazine carbon nanotubes for pretargeted in vivo “Click on-to-Launch” bioorthogonal tumour imaging. Angew. Chem. 59, 16023–16032 (2020).
Srinivasan, S. et al. SQ3370 prompts cytotoxic drug through click on chemistry at tumor and elicits sustained responses in injected and non-injected lesions. Adv. Ther. 4, 2000243 (2021).
Lu, W.-Y., Lu, W.-Y., Hen, T. & Forbes, S. Isolation and growth of the hepatic progenitor cell (HPC) inhabitants. Protoc. Exch. (2015).
Vincent, V. et al. A novel circulation cytometry-based quantitative monocyte adhesion assay to estimate endothelial cell activation in vitro. BioTechniques 68, 325–333 (2020).