A brand new sort of allogeneic CAR-T cell immunotherapy that targets aggressive blood cancers has proven promising outcomes alongside manageable negative effects, in response to the outcomes of a world Section 1/2 medical trial led by researchers at Washington College College of Drugs in St. Louis.
The dose-escalating medical trial evaluated the security and efficacy of the CAR-T cell remedy WU-CART-007, which is particularly designed to assault cancerous T cells, in 28 contributors identified with T cell acute lymphoblastic leukemia (T-ALL) or T cell lymphoblastic lymphoma (T-LBL). The trial contributors had run out of remedy choices after customary remedy proved ineffective. The reported examine outcomes confirmed that a lot of the sufferers who obtained the total dose of the brand new immunotherapy achieved full remission of their most cancers.
“For sufferers with these uncommon and aggressive cancers, who haven’t any different choices, this has the potential to change into a transformative advance within the discipline,” mentioned John F. DiPersio, MD, PhD, the Virginia E. & Sam J. Golman Professor of Drugs at WashU Drugs, who first developed the remedy in his lab. “The trial demonstrated a excessive probability of response to the remedy and even remission. Whereas bigger research with extra sufferers and longer follow-up are crucial earlier than the researchers can decide whether or not this new remedy might be healing by itself, DiPersio commented, “this CAR-T cell remedy reveals promise in turning into a ‘bridge-to-transplant’ remedy for sufferers who would in any other case not be eligible for stem cell transplantation, which is the one doubtlessly healing remedy for these blood cancers.”
DiPersio is senior writer of the group’s printed report in Blood, titled “Section 1/2 Trial of Anti-CD7 allogeneic WU-CART-007 in sufferers with relapsed/refractory T-cell malignancies.” Whereas acknowledging that interpretation of their examine outcomes is restricted by small pattern dimension and lack of a comparator arm, the investigators concluded, “This program has the potential to advance an off-the-shelf allogenic CAR-T cell remedy and supply a brand new remedy choice for relapsed CD7-positive T-cell malignancies comparable to T-ALL/LBL, which characterize a big unmet medical want.”
“Relapsed/refractory (R/R) T-cell acute lymphoblastic leukemia (T-ALL) and lymphoblastic lymphoma (T-LBL) carry a dismal prognosis with restricted efficient therapeutic choices,” the authors wrote. Normal chemotherapy remedy leads to “poor final result,” and the median general survival is simply 6 months amongst individuals who reply. WHO classifies T-ALL and T-LBL as the identical illness, the authors famous, and the medical method to remedy of each is comparable. “There isn’t a customary of care remedy for grownup sufferers with relapsed illness,” they famous, “.. thus, there’s an unmet medical want …” About 1,000 individuals are identified with these cancers yearly within the U.S. If the most cancers doesn’t reply to remedy or returns after preliminary remedy, sufferers survive on common solely six months, and fewer than 7% surviving to the five-year mark.” No remedy moreover nelarabine has been permitted on this setting since 2005, with unsatisfactory response charges,” the investigators continued.
Generated from CRISPR-edited wholesome donor T cells, WU-CART-007 is an allogeneic CD7-directed, genetically modified, fratricide-resistant CAR-T cell product that’s beneath growth for treating CD7-positive hematologic malignancies. “Proof-of-concept of this method, allogeneic-sourced CD7 focusing on CAR-T cells, has been beforehand reported in small single website research,” the researchers famous.
The newly reported trial included 28 grownup and adolescent sufferers with T cell acute lymphoblastic leukemia and T cell lymphoblastic lymphoma that both returned after a number of traces of remedy or that didn’t reply to preliminary remedy. The examine was performed in Australia, Europe and a number of websites throughout the U.S. For the St. Louis website, the trial was performed at Siteman Most cancers Middle, primarily based at Barnes-Jewish Hospital and WashU Drugs.
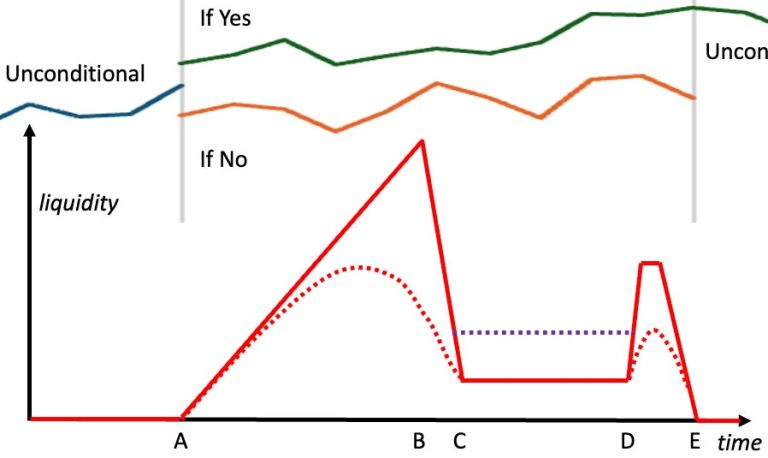
The trial design included a dose-escalation section, which decided the really useful dose of therapeutic cells that sufferers would obtain for the second section of the trial. Dose escalation helps decide the biggest dose of CAR-T cells that sufferers can obtain and nonetheless have manageable negative effects. 13 sufferers obtained the total really useful section 2 dose (RP2D) of 900 million CAR-T cells after present process a process to clear their very own immune cells. This process, referred to as lymphodepletion, reduces immune cells, making room for the brand new therapeutic T cells to ascertain themselves and develop in quantity. Two of those sufferers died from their most cancers or remedy problems, comparable to an infection, through the examine interval.
Of 11 sufferers who might be evaluated after remedy, the general response fee was 90.9%, that means 10 sufferers both confirmed no indicators of most cancers after remedy or their most cancers cell burden was diminished considerably. Eight out of 11 sufferers (72.7%) achieved full remission. On the examine’s knowledge reduce off, six sufferers who underwent a transplant stay in remission, with no proof of illness, six to 12 months later.
“These response and remission charges—starting from 70%-90% of sufferers—are a lot increased than we’d count on from standard-of-care for this most cancers sort, which generally results in remission in solely 20%-40% of sufferers,” mentioned first and corresponding writer Armin Ghobadi, MD, a professor of medication and medical director of the Middle for Gene and Mobile Immunotherapy at WashU Drugs. “These responses are exceptional as a result of the sufferers on this trial had run out of choices. They’d very aggressive cancers return after a number of traces of remedy, together with a number of who relapsed after an earlier stem cell transplant.”
Most sufferers (88.5%) skilled cytokine launch syndrome as a aspect impact of the immunotherapy, and these circumstances have been predominantly gentle or reasonable. Cytokine launch syndrome is a typical aspect impact of CAR-T cell remedy that happens when giant numbers of immune cells launch chemical compounds that trigger a full-body inflammatory response. About 19% of the sufferers skilled more-severe cytokine launch syndrome. A small variety of sufferers skilled rarer negative effects, comparable to neurotoxicity syndrome and low-grade graft-versus-host illness. Hostile occasions have been managed with further therapies. Of their paper, the authors acknowledged, “WU-CART-007 on the RP2D demonstrated a excessive response fee in sufferers with relapsed/refractory T-ALL/LBL and has the potential to offer a brand new remedy choice.”
The immunotherapy evaluated within the trial is taken into account a “common” CAR-T cell remedy as a result of—harnessing CRISPR gene modifying expertise—it may be produced from cells donated by any wholesome particular person and used to deal with any affected person with a T cell most cancers. In distinction, permitted CAR-T cell therapies are tailored from the affected person’s immune cells. The cells have to be collected from the affected person and shipped to a producing facility to be made after which shipped again, a course of that sometimes takes three to 6 weeks. In distinction, common CAR-T cell therapies will be made forward of time, saved frozen and be available “off-the-shelf,” tremendously decreasing the wait time earlier than remedy can start.
Utilizing CRISPR gene modifying instruments, the manufacturing course of deletes the T cell receptor from the donor cells, tremendously decreasing the chance of graft-versus-host illness, by which donor T cells assault wholesome tissue. Eradicating one other key antigen additionally prevents the CAR-T cells from attacking each other. The varieties of uncommon cancers on this examine introduced a novel problem: the therapeutic cells and the most cancers cells are each T cells, so steps have to be taken to stop the therapeutic T cells from mistaking each other for the most cancers and inflicting CAR-T cell fratricide. All different permitted CAR-T cell therapies goal B cell cancers, which shouldn’t have this T cell self-targeting complication.
After utilizing CRISPR gene modifying to change the CAR-T cells to stop these dangerous negative effects, the cells are additional engineered to focus on a protein referred to as CD7 on the floor of cancerous T cells to then destroy the most cancers. In abstract, the authors wrote, “To fabricate WU-CART-007 drug product, T cells generated from wholesome donors are CRISPR-Cas9 edited to delete CD7 and T-cell receptor alpha fixed gene (TRAC), transduced with a second-generation CAR focusing on CD7, expanded, purified to take away residual T-cell receptor ⍺/β-positive cells, and cryopreserved.”
WU-CART-007 is in growth by Wugen, a WashU biotech startup firm based by DiPersio and different WashU Drugs investigators, together with co-author Matthew Cooper, PhD, who cofounded the corporate when he was on the WashU Drugs college and now serves as Wugen’s chief scientific officer. “A bigger worldwide medical trial of this remedy is already underway,” DiPersio mentioned. “We should full this bigger trial first, however we’re hopeful this common CAR-T cell remedy can change into an permitted remedy for sufferers with lethal T cell cancers.”