Downing, Ok. et al. Previous and new biomarkers for volumetric muscle loss. Curr. Opin. Pharm. 59, 61–69 (2021).
Corona, B. T., Rivera, J. C. & Greising, S. M. Inflammatory and physiological penalties of debridement of fibrous tissue after volumetric muscle loss harm. Clin. Transl. Sci. 11, 208–217 (2018).
Grasman, J. M., Zayas, M. J., Web page, R. L. & Pins, G. D. Biomimetic scaffolds for regeneration of volumetric muscle loss in skeletal muscle accidents. Acta Biomater. 25, 2–15 (2015).
Lakhiani, C., DeFazio, M., Han, Ok., Falola, R. & Evans, Ok. Donor-site morbidity following free tissue harvest from the thigh: a scientific evaluate and pooled evaluation of issues. J. Reconstr. Microsurg. 32, 342–357 (2016).
Lee, Ok.-T. & Mun, G.-H. A scientific evaluate of practical donor-site morbidity after latissimus dorsi muscle switch. Plast. Reconstr. Surg. 134, 303–314 (2014).
Bianchi, B., Copelli, C., Ferrari, S., Ferri, A. & Sesenna, E. Free flaps: outcomes and issues in head and neck reconstructions. J. Cranio Maxillofac. Surg. 37, 438–442 (2009).
Garg, Ok. et al. Volumetric muscle loss: persistent practical deficits past frank lack of tissue. J. Orthop. Res. 33, 40–46 (2015).
Mase, V. J. et al. Medical utility of an acellular biologic scaffold for surgical restore of a big, traumatic quadriceps femoris muscle defect. Orthopedics 33, 511 (2010).
Dziki, J. L., Sicari, B. M., Wolf, M. T., Cramer, M. C. & Badylak, S. F. Immunomodulation and mobilization of progenitor cells by extracellular matrix bioscaffolds for volumetric muscle loss remedy. Tissue Eng. Half A 22, 1129–1139 (2016).
Sicari, B. M. et al. An acellular biologic scaffold promotes skeletal muscle formation in mice and people with volumetric muscle loss. Sci. Transl. Med. 6, 234ra58 (2014).
Pham‐Nguyen, O. et al. Preparation of stretchable nanofibrous sheets with sacrificial coaxial electrospinning for remedy of traumatic muscle harm. Adv. Healthc. Mater. 10, 2002228 (2021).
Jia, W. et al. Glass-activated regeneration of volumetric muscle loss. Acta Biomater. 103, 306–317 (2020).
Jeong, G.-J., Castels, H., Kang, I., Aliya, B. & Jang, Y. C. Nanomaterial for skeletal muscle regeneration. Tissue Eng. Regen. Med. 19, 253–261 (2022).
Ge, J. et al. Gold and gold-silver alloy nanoparticles improve the myogenic differentiation of myoblasts by way of p38 MAPK signaling pathway and promote in vivo skeletal muscle regeneration. Biomaterials 175, 19–29 (2018).
Kim, S. J. et al. Stretchable and clear biointerface utilizing cell‐sheet–graphene hybrid for electrophysiology and remedy of skeletal muscle. Adv. Funct. Mater. 26, 3207–3217 (2016).
Ge, J. et al. Engineering conductive antioxidative antibacterial nanocomposite hydrogel scaffolds with oriented channels promotes structure-functional skeletal muscle regeneration. Chem. Eng. J. 425, 130333 (2021).
Kim, W., Jang, C. H. & Kim, G. H. A myoblast-laden collagen bioink with totally aligned au nanowires for muscle-tissue regeneration. Nano Lett. 19, 8612–8620 (2019).
Nakayama, Ok. H. et al. Remedy of volumetric muscle loss in mice utilizing nanofibrillar scaffolds enhances vascular group and integration. Commun. Biol. 2, 170 (2019).
Russell, C. S. et al. In situ printing of adhesive hydrogel scaffolds for the remedy of skeletal muscle accidents. ACS Appl. Bio Mater. 3, 1568–1579 (2020).
Fornetti, E. et al. A novel extrusion-based 3D bioprinting system for skeletal muscle tissue engineering. Biofabrication 15, 025009 (2023).
Li, T. et al. Bioprinted anisotropic scaffolds with quick stress leisure bioink for engineering 3D skeletal muscle and repairing volumetric muscle loss. Acta Biomater. 156, 21–36 (2023).
Gilbert-Honick, J. et al. Engineering 3D skeletal muscle primed for neuromuscular regeneration following volumetric muscle loss. Biomaterials 255, 120154 (2020).
Haas, G. J. et al. Biomimetic sponges for regeneration of skeletal muscle following trauma. J. Biomed. Mater. Res Half A 107, 92–103 (2019).
Haas, G. et al. Biomimetic sponges enhance muscle construction and performance following volumetric muscle loss. J. Biomed. Mater. Res. 109, 2280–2293 (2021).
Eugenis, I. et al. Scalable macroporous hydrogels improve stem cell remedy of volumetric muscle loss. Biomaterials 290, 121818 (2022).
Tanner, G. I., Schiltz, L., Narra, N., Figueiredo, M. L. & Qazi, T. H. Granular hydrogels enhance myogenic invasion and restore after volumetric muscle loss. Adv. Healthc. Mater. 13, e2303576 (2024).
Greising, S. M., Corona, B. T., McGann, C., Frankum, J. Ok. & Warren, G. L. Therapeutic approaches for volumetric muscle loss harm: a scientific evaluate and meta-analysis. Tissue Eng. Half B Rev. https://doi.org/10.1089/ten.teb.2019.0207 (2019).
Blakney, A. Ok., Swartzlander, M. D. & Bryant, S. J. The consequences of substrate stiffness on the in vitro activation of macrophages and in vivo host response to poly(ethylene glycol)-based hydrogels. J. Biomed. Mater. Res. 100A, 1375–1386 (2012).
Swartzlander, M. D. et al. Linking the international physique response and protein adsorption to PEG-based hydrogels utilizing proteomics. Biomaterials 41, 26–36 (2015).
Vegas, A. J. et al. Combinatorial hydrogel library permits identification of supplies that mitigate the international physique response in primates. Nat. Biotechnol. 34, 345–352 (2016).
Zhang, L. et al. Zwitterionic hydrogels implanted in mice resist the foreign-body response. Nat. Biotechnol. 31, 553–556 (2013).
Cha, B.-H. et al. Integrin-mediated interactions management macrophage polarization in 3D hydrogels. Adv. Well being. Mater. 6, 1700289 (2017).
García, J. R. et al. IFN-γ-tethered hydrogels improve mesenchymal stem cell-based immunomodulation and promote tissue restore. Biomaterials 220, 119403 (2019).
Vasconcelos, D. P. et al. Modulation of the inflammatory response to chitosan by way of M2 macrophage polarization utilizing pro-resolution mediators. Biomaterials 37, 116–123 (2015).
Von den Hoff, J. W., Carvajal Monroy, P. L., Ongkosuwito, E. M., van Kuppevelt, T. H. & Daamen, W. F. Muscle fibrosis within the taste bud: supply of cells, development components and anti-fibrotics. Adv. Drug Deliv. Rev. 146, 60–76 (2019).
DiEgidio, P. et al. Biomedical implant capsule formation: classes discovered and the highway forward. Ann. Plast. Surg. 73, 451–460 (2014).
Morais, J. M., Papadimitrakopoulos, F. & Burgess, D. J. Biomaterials/tissue interactions: potential options to beat international physique response. AAPS J. 12, 188–196 (2010).
Veiseh, O. & Vegas, A. J. Domesticating the international physique response: current advances and functions. Adv. Drug Deliv. Rev. 144, 148–161 (2019).
Fayzullin, A. et al. Native supply of pirfenidone by PLA implants modifies international physique response and prevents fibrosis. Biomedicines 9, 853 (2021).
Sussman, E. M., Halpin, M. C., Muster, J., Moon, R. T. & Ratner, B. D. Porous implants modulate therapeutic and induce shifts in native macrophage polarization within the international physique response. Ann. Biomed. Eng. 42, 1508–1516 (2014).
Bryers, J. D., Giachelli, C. M. & Ratner, B. D. Engineering biomaterials to combine and heal: the biocompatibility paradigm shifts. Biotechnol. Bioeng. 109, 1898–1911 (2012).
Corona, B. T. et al. The promotion of a practical fibrosis in skeletal muscle with volumetric muscle loss harm following the transplantation of muscle-ECM. Biomaterials 34, 3324–3335 (2013).
Dolan, C. P. et al. Evaluating the potential use of practical fibrosis to facilitate improved outcomes following volumetric muscle loss harm. Acta Biomater. 140, 379–388 (2022).
Li, L., Xiong, W.-C. & Mei, L. Neuromuscular junction formation, growing older, and issues. Annu Rev. Physiol. 80, 159–188 (2018).
Sirago, G., Pellegrino, M. A., Bottinelli, R., Franchi, M. V. & Narici, M. V. Lack of neuromuscular junction integrity and muscle atrophy in skeletal muscle disuse. Ageing Res. Rev. 83, 101810 (2023).
Vannucci, B. et al. What’s Regular? Neuromuscular junction reinnervation after nerve harm. Muscle Nerve 60, 604–612 (2019).
Sorensen, J. R., Hoffman, D. B., Corona, B. T. & Greising, S. M. Secondary denervation is a persistent pathophysiologic sequela of volumetric muscle loss. J. Appl. Physiol. 130, 1614–1625 (2021).
Hoffman, D. B. et al. Response of terminal Schwann cells following volumetric muscle loss harm. Exp. Neurol. 365, 114431 (2023).
Wu, J., Matthias, N., Bhalla, S. & Darabi, R. Analysis of the therapeutic potential of human iPSCs in a murine mannequin of VML. Mol. Ther. 29, 121–131 (2021).
Genovese, P. et al. Co‐supply of fibrin‐laminin hydrogel with mesenchymal stem cell spheroids helps skeletal muscle regeneration following trauma. J. Tissue Eng. Regen. Med. 15, 1131–1143 (2021).
Das, S. et al. Pre-innervated tissue-engineered muscle promotes a pro-regenerative microenvironment following volumetric muscle loss. Commun. Biol. 3, 330 (2020).
Rodriguez, B. L. et al. A tissue engineering strategy for repairing craniofacial volumetric muscle loss in a sheep following a 2, 4, and 6-month restoration. PLoS ONE 15, e0239152 (2020).
Nakayama, Ok. H. et al. Rehabilitative train and spatially patterned nanofibrillar scaffolds improve vascularization and innervation following volumetric muscle loss. npj Regen. Med. 3, 16 (2018).
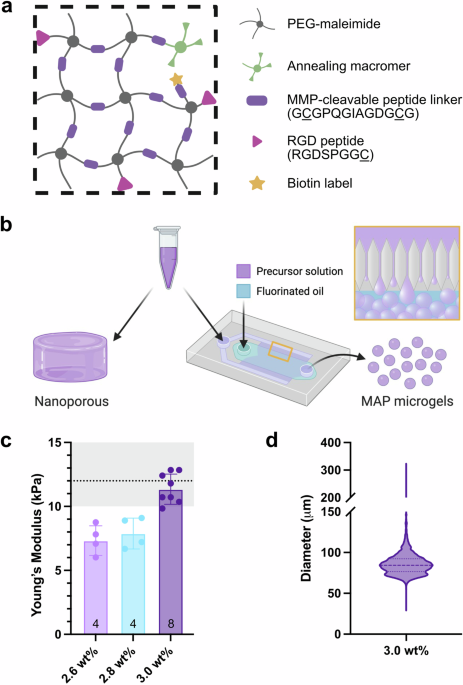
Pruett, L. J., Jenkins, C. H., Singh, N. S., Catallo, Ok. J. & Griffin, D. R. Heparin microislands in microporous annealed particle scaffolds for accelerated diabetic wound therapeutic. Adv. Funct. Mater. 31, 2104337 (2021).
Pruett, L., Ellis, R., McDermott, M., Roosa, C. & Griffin, D. Spatially heterogeneous epidermal development issue launch from microporous annealed particle (MAP) hydrogel for improved wound closure. J. Mater. Chem. B 9, 7132–7139 (2021).
Nih, L. R., Sideris, E., Carmichael, S. T. & Segura, T. Injection of microporous annealing particle (MAP) hydrogels within the stroke cavity reduces gliosis and irritation and promotes NPC migration to the lesion. Adv. Mater. 29, 1606471 (2017).
Sideris, E. et al. Particle hydrogels lower cerebral atrophy and attenuate astrocyte and microglia/macrophage reactivity after stroke. Adv. Ther. 5, 2200048 (2022).
Fang, J. et al. Injectable drug‐releasing microporous annealed particle scaffolds for treating myocardial infarction. Adv. Funct. Mater. 30, 2004307 (2020).
Pruett, L. et al. Improvement of a microporous annealed particle hydrogel for lengthy‐time period vocal fold augmentation. Laryngoscope 130, 2432–2441 (2020).
Pruett, L. J. et al. De novo tissue formation utilizing customized microporous annealed particle hydrogel gives long-term vocal fold augmentation. npj Regen. Med. 8, 10 (2023).
Schaeffer, C. et al. Injectable microannealed porous scaffold for articular cartilage regeneration. Ann. Plast. Surg. 84, S446–S450 (2020).
Ross, B. C. et al. Constructing-Block measurement mediates microporous annealed particle hydrogel tube microenvironment following spinal twine harm. Adv. Healthc. Mater. 13, 2302498 (2023).
Koh, J. et al. Enhanced in vivo supply of stem cells utilizing microporous annealed particle scaffolds. Small 15, 1903147 (2019).
Griffin, D. R., Weaver, W. M., Scumpia, P. O., Di Carlo, D. & Segura, T. Accelerated wound therapeutic by injectable microporous gel scaffolds assembled from annealed constructing blocks. Nat. Mater. 14, 737–744 (2015).
Liu, Y. et al. Spatial confinement modulates macrophage response in microporous annealed particle (MAP) scaffolds. Adv. Well being. Mater. 12, 2300823 (2023).
Pfaff, B. N. et al. Selective and improved photoannealing of microporous annealed particle (MAP) scaffolds. ACS Biomater. Sci. Eng. 7, 422–427 (2021).
de Rutte, J. M., Koh, J. & Carlo, D. D. Scalable high-throughput manufacturing of modular microgels for in situ meeting of microporous tissue scaffolds. Adv. Funct. Mater. 29, 1900071 (2019).
Engler, A. J. et al. Myotubes differentiate optimally on substrates with tissue-like stiffness: pathological implications for comfortable or stiff microenvironments. J. Cell Biol. 166, 877–887 (2004).
Laumonier, T. & Menetrey, J. Muscle accidents and techniques for bettering their restore. J. Exp. Ortop. 3, 15 (2016).
Corona, B. T., Ward, C. L., Baker, H. B., Walters, T. J. & Christ, G. J. Implantation of in vitro tissue engineered muscle restore constructs and bladder acellular matrices partially restore in vivo skeletal muscle perform in a rat mannequin of volumetric muscle loss harm. Tissue Eng. Half A 20, 705–715 (2013).
Wu, X., Corona, B. T., Chen, X. & Walters, T. J. A standardized rat mannequin of volumetric muscle loss harm for the event of tissue engineering therapies. Biores. Open Entry 1, 280–290 (2012).
Tidball, J. G. & Villalta, S. A. Regulatory interactions between muscle and the immune system throughout muscle regeneration. Am. J. Physiol. Regul. Integr. Comp. Physiol. 298, R1173–R1187 (2010).
Kowal, Ok. et al. CD163 and its function in irritation. Folia Histochem. Cytobiol. 49, 365–374 (2011).
Deng, B., Wehling-Henricks, M., Villalta, S. A., Wang, Y. & Tidball, J. G. IL-10 triggers adjustments in macrophage phenotype that promote muscle development and regeneration. J. Immunol. 189, 3669–3680 (2012).
Massimino, M. L. et al. ED2+ macrophages improve selectively myoblast proliferation in muscle cultures. Biochem. Biophys. Res. Commun. 235, 754–759 (1997).
Latroche, C. et al. Skeletal muscle microvasculature: a extremely dynamic lifeline. Physiology 30, 417–427 (2015).
Kusters, Y. H. A. M. & Barrett, E. J. Muscle microvasculature’s structural and practical specializations facilitate muscle metabolism. Am. J. Physiol. Endocrinol. Metab. 310, E379–E387 (2016).
Sarveswaran, Ok. et al. Artificial capillaries to regulate microscopic blood circulation. Sci. Rep. 6, 21885 (2016).
Corona, B. T. et al. Impression of volumetric muscle loss harm on persistent motoneuron axotomy. Muscle Nerve 57, 799–807 (2018).
Wu, P. et al. Key adjustments in denervated muscular tissues and their influence on regeneration and reinnervation. Neural Regen. Res. 9, 1796 (2014).
Carré, D. et al. The distribution of neuromuscular junctions will depend on muscle pennation, when botulinum neurotoxin receptors and SNAREs expression are uniform within the rat. Toxicon 212, 34–41 (2022).
Feinberg, A. W. et al. Controlling the contractile power of engineered cardiac muscle by hierarchal tissue structure. Biomaterials 33, 5732–5741 (2012).
Grosberg, A. et al. Self-organization of muscle cell construction and performance. PLoS Comput. Biol. 7, e1001088 (2011).
Passipieri, J. A. et al. Keratin hydrogel enhances in vivo skeletal muscle perform in a rat mannequin of volumetric muscle loss. Tissue Eng. Half A 23, 556–571 (2017).
Rosas-Arellano, A. et al. A easy resolution for antibody sign enhancement in immunofluorescence and triple immunogold assays. Histochem. Cell Biol. 146, 421–430 (2016).
Stirling, D. R. et al. CellProfiler 4: enhancements in pace, utility and value. BMC Bioinform. 22, 433 (2021).
Bankhead, P. et al. QuPath: open supply software program for digital pathology picture evaluation. Sci. Rep. 7, 16878 (2017).